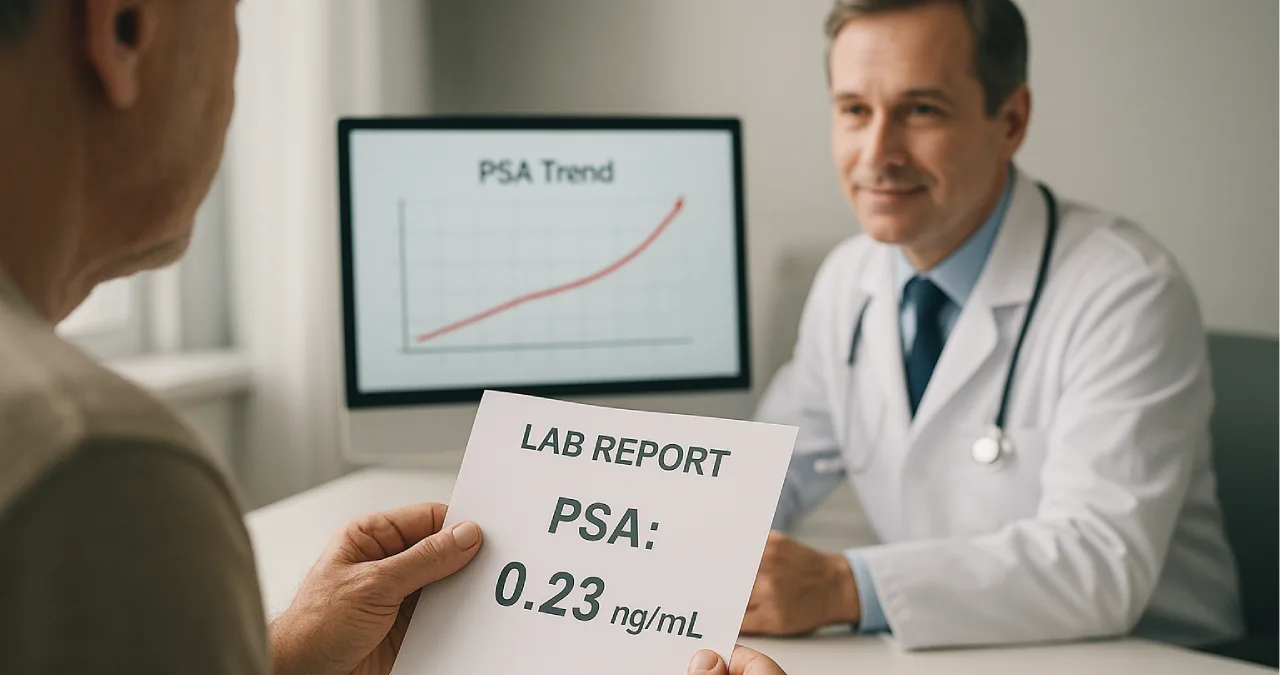
You had your prostate removed, and you expect your PSA to drop to zero. Then suddenly, a small number appears on your report — maybe 0.1, 0.17, or even 0.23. Your mind goes straight to the worst-case scenario.
You’re not alone.
Thousands of men search every month:
“What is a dangerous PSA level after prostate removal?”
This guide breaks down the answer clearly — no jargon, no confusion — just practical information you can actually use.
What is PSA? A Quick Refresher
PSA: The Protein and the Test
PSA (Prostate-Specific Antigen) is a protein produced by prostate cells. Before surgery, PSA can be elevated for many reasons — cancer, inflammation, infection, or benign enlargement.
How PSA Behaves Before vs After Surgery
Once the prostate is completely removed (radical prostatectomy):
- The organ producing PSA is gone
- PSA levels should drop to almost zero
- Any detectable PSA after healing is a red flag that needs evaluation
After prostate removal, PSA acts as a “warning light” for possible cancer activity.
What to Expect After Radical Prostatectomy
“Undetectable PSA” — What Doctors Mean
Most men reach undetectable PSA (<0.1 ng/mL) within:
- 6–8 weeks after surgery
- Nearly all within 3 months
This “undetectable” level is the new baseline.
PSA Timeline After Surgery
- Weeks 1–8 → PSA drops extremely low
- 2–3 months → PSA reaches its lowest point (nadir)
- Beyond 3 months → PSA should remain undetectable or extremely close to zero
If PSA becomes detectable later, doctors evaluate for recurrence.
What Is a Dangerous PSA Level After Prostate Removal?
Biochemical Recurrence (BCR) — The Standard Definition
Doctors consider PSA “dangerous” when it meets the widely used recurrence threshold:
A PSA level of ≥ 0.2 ng/mL, confirmed with a second test
This is called Biochemical Recurrence (BCR) — meaning prostate cancer cells may be active again.
Persistent PSA vs Recurrent PSA
These two are very different:
1. Persistent PSA
- Your PSA never becomes undetectable after surgery.
- Suggests there was already cancer outside the prostate at removal time or leftover tissue.
2. Recurrent PSA
- PSA was undetectable after surgery
- Then begins to rise later
- This is classic biochemical recurrence
Understanding which category you fall into helps guide treatment.
Numbers That Matter — PSA Threshold Breakdown
PSA Less Than 0.1 ng/mL — Ideal and Expected
This range is considered:
- Undetectable
- Normal post-prostatectomy
- Not a cause for concern
If your PSA stays below 0.1 ng/mL, you’re doing well.
PSA 0.1–0.19 ng/mL — The “Gray Zone”
This range triggers watchful waiting, not immediate treatment.
Doctors often:
- Repeat PSA in a few weeks
- Monitor trends
- Evaluate timing (early after surgery vs years later)
A single reading here is not automatically dangerous.
PSA ≥ 0.2 ng/mL — The Warning Point
A PSA of 0.2 ng/mL or higher, confirmed by another test, is considered:
- Biochemical recurrence
- A sign that cancer may have returned or persisted
- A trigger for imaging and treatment discussions
But this does not mean the cancer has spread — only that further evaluation is needed.
Why a Confirmatory PSA Test Matters
A second test is essential because:
- PSA can fluctuate
- Lab variations occur
- Stress, activity, or transient inflammation can cause tiny bumps
Doctors confirm to avoid unnecessary panic and overtreatment.
Is a Single Low PSA Jump Dangerous?
Why Trends Matter More Than One Value
A one-off reading like 0.11 ng/mL does not automatically equal recurrence.
What matters more is the pattern over time.
Doctors check:
- Is PSA rising consistently?
- How quickly is it rising?
- How many consecutive increases occur?
PSA Doubling Time (PSA-DT)
This is one of the most important predictors.
- Short doubling time (fast rise) → Higher concern
- Long doubling time (slow rise) → More time to monitor
A PSA-DT of less than 6 months is more concerning and often triggers early treatment plans.
What Doctors Do When PSA Becomes Detectable
PSMA PET/CT Scan — Modern Imaging for Recurrence
This imaging scan detects extremely small cancer deposits.
Doctors usually recommend it when:
- PSA rises above 0.2 ng/mL
- PSA continues rising steadily
- PSA doubling time becomes short
It helps locate recurrence:
- Local (prostate bed)
- Regional (lymph nodes)
- Distant (bones or organs)
Salvage Radiotherapy (SRT)
This is the most common treatment for recurrent PSA.
Doctors prefer starting SRT when PSA is:
≤ 0.5 ng/mL (ideally around 0.2–0.3)
Earlier treatment = better long-term control.
Hormone Therapy (ADT)
In some cases, doctors combine:
- Salvage radiotherapy
- Short-term hormone therapy
This enhances effectiveness for higher-risk cancers.
Risk Factors That Change What Counts as “Dangerous”
Some men need earlier or more aggressive action even at lower PSA levels.
Higher risk factors include:
- High Gleason score / Grade Group
- Positive surgical margins
- Invasion outside the prostate
- High PSA before surgery
- Fast-rising PSA
- Family history
- Younger age (longer life expectancy)
These factors guide how quickly your doctor responds to rising PSA.
Practical Monitoring Plan After Prostate Removal
Standard PSA Testing Schedule
Typical follow-up includes:
- Every 3–4 months for the first year
- Every 6 months during years 2–3
- Once per year afterward (if stable)
High-risk patients may test more frequently.
What to Do If Your PSA Rises
- Repeat PSA to confirm
- Check PSA doubling time
- Discuss early PSMA PET/CT
- Consider salvage radiotherapy early
- Evaluate if hormone therapy is needed
- Stay consistent with monitoring
Emotional and Practical Considerations
PSA Anxiety is Real
Watching PSA levels can feel like watching a bomb timer.
You’re not imagining it — many men struggle with “PSA anxiety.”
Creating a plan with your doctor helps regain control.
Questions to Ask Your Doctor
- What does my PSA trend show?
- Should I repeat the test sooner?
- When should we consider PSMA scanning?
- What are my salvage treatment options?
- What are the risks and benefits?
- How fast is my PSA doubling?
Common Myths About PSA After Prostate Removal
Myth 1: Any detectable PSA means cancer has spread
Truth:
Small PSA amounts can come from benign tissue remnants.
Myth 2: A high PSA always means worse outcomes
Truth:
PSA trend, not just value, determines risk.
Real-World Outcomes — What the Data Shows
Early Salvage Treatment Works
Studies show that treating recurrence early (low PSA levels) increases chances of:
- Long-term remission
- Better survival
- Fewer complications
Long-Term Survival
Many men live decades after recurrence when it’s caught early and treated appropriately.
Conclusion
A dangerous PSA level after prostate removal is typically defined as a confirmed PSA of 0.2 ng/mL or higher. But numbers alone don’t tell the whole story. Trends, doubling time, pathology, and timing all matter just as much.
Staying consistent with PSA monitoring, understanding your personal risk factors, and discussing early intervention with your doctor are the keys to staying ahead of recurrence.
Knowledge = control.
Monitoring = safety.
Early detection = better outcomes.
FAQs
Not usually. Doctors typically repeat the test and watch the trend before making decisions.
A confirmed PSA of ≥ 0.2 ng/mL meets the common definition of biochemical recurrence.
Often recommended when PSA rises above 0.2 ng/mL or shows a rapid doubling time.
Yes, but outcomes are best when PSA is ≤ 0.5 ng/mL at the time of treatment.
Usually every 3–4 months in year 1, every 6 months in years 2–3, and yearly thereafter.